Struggling with engorged breasts while breastfeeding? 😊 This guide explains why engorgement happens, offers simple relief tips like warm compresses and frequent nursing, and shares prevention strategies. Find expert advice and visuals to ease discomfort fast!
Hey, mamas! 😄 I’m a mom running BestBabyCart.com, and I remember those early breastfeeding days when my breasts felt like overfilled water balloons—ouch! Engorgement is common, but it can feel overwhelming. Questions like “Why are my breasts so hard?” or “How do I get relief?” pop up fast. Don’t worry—this mom-to-mom guide on how to manage engorgement breastfeeding has you covered. With practical tips, soothing visuals, and trusted advice, you’ll find comfort and confidence. Let’s tackle engorgement together!
What Is Breast Engorgement?
Engorgement happens when your breasts become overly full of milk, making them hard, swollen, and painful. It’s common in the first 3–5 days after birth as your milk “comes in,” per La Leche League, but can occur later too.
-
Why It Happens: Milk supply increases to meet baby’s demand, or missed feedings cause buildup.
-
Why It Matters: Understanding the cause helps you find relief.
-
-
Symptoms: Tight, shiny skin; warm, heavy breasts; flattened nipples.
-
Why It Matters: Recognizing signs lets you act quickly.
-
-
How Long It Lasts: Usually 24–48 hours with proper management.
-
Why It Matters: Relief is near with the right steps!
-
About 1 in 3 breastfeeding moms experience engorgement, per CDC, so you’re not alone. Let’s explore how to ease the discomfort!
Why Does Engorgement Happen?
Understanding the causes helps you manage and prevent engorgement. Here are the main triggers:
Milk Supply Transition
-
When: Days 3–5 postpartum, milk shifts from colostrum to mature milk.
-
Why It Matters: Sudden milk surge fills breasts faster than baby can drink.
-
-
How It Feels: Breasts feel rock-hard and tender.
-
Why It Matters: Signals your body’s adjusting to breastfeeding.
-
Missed or Irregular Feedings
-
When: Baby sleeps longer, or you skip pumping.
-
Why It Matters: Milk builds up, causing pressure.
-
-
Example: Missing a night feed when baby sleeps 6 hours.
-
Why It Matters: Helps you plan feeding schedules.
-
Weaning or Reduced Nursing
-
When: Baby starts solids or you wean.
-
Why It Matters: Less milk removal leads to fullness.
-
-
How to Avoid: Gradually reduce feedings, per American Academy of Pediatrics.
-
Why It Matters: Slow changes prevent engorgement.
-
Other Factors
-
Blocked Ducts: Milk flow gets stuck, causing swelling.
-
Why It Matters: Needs attention to avoid mastitis.
-
-
Overstimulation: Too much pumping increases supply.
-
Why It Matters: Balance pumping with baby’s demand.
-

How Does It Feel?
Engorgement can make your breasts feel:
- Hard or tight
- Warm or hot to the touch
- Painful or tender
- Heavy, with stretched, shiny skin
- You might also notice flattened nipples, making it harder for your baby to latch.
Prevention Strategies
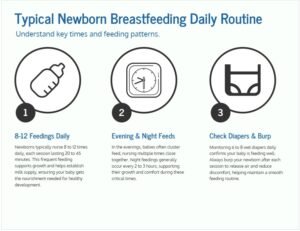
Breast engorgement can be a painful challenge for new mothers. Preventing it is crucial for comfort and health. Effective strategies can help manage this condition before it worsens. These methods focus on feeding routines and proper latch techniques.
How to Relieve Engorgement Fast
Engorgement hurts, but these expert-backed tips bring relief. Try these methods to feel better:
Nurse or Pump Frequently
-
How: Feed baby every 2–3 hours or pump with a Medela pump.
-
Why It Works: Removes milk, reducing pressure.
-
-
Tip: Wake baby for feeds if they sleep long, per HealthyChildren.org.
-
Why It Helps: Keeps milk flowing.
-
Use Warm Compresses Before Feeding
-
How: Apply a warm, wet cloth or Lansinoh hot/cold pack for 5–10 minutes.
-
Why It Works: Softens breasts, eases milk flow.
-
-
Caution: Avoid too much heat to prevent burns.
-
Why It Helps: Ensures safe relief.
-
Massage Breasts Gently
-
How: Use circular motions toward the nipple while nursing.
-
Why It Works: Clears blocked ducts, per La Leche League.
-
-
Tip: Massage during a warm shower for extra comfort.
-
Why It Helps: Combines heat and touch for relief.
-
Cold Compresses After Feeding
-
How: Use a cold Lansinoh pack or chilled cabbage leaves for 15 minutes.
-
Why It Works: Reduces swelling and pain.
-
-
Fun Fact: Cabbage leaves have natural anti-inflammatory properties!
-
Why It Helps: Offers a natural, soothing option.
-
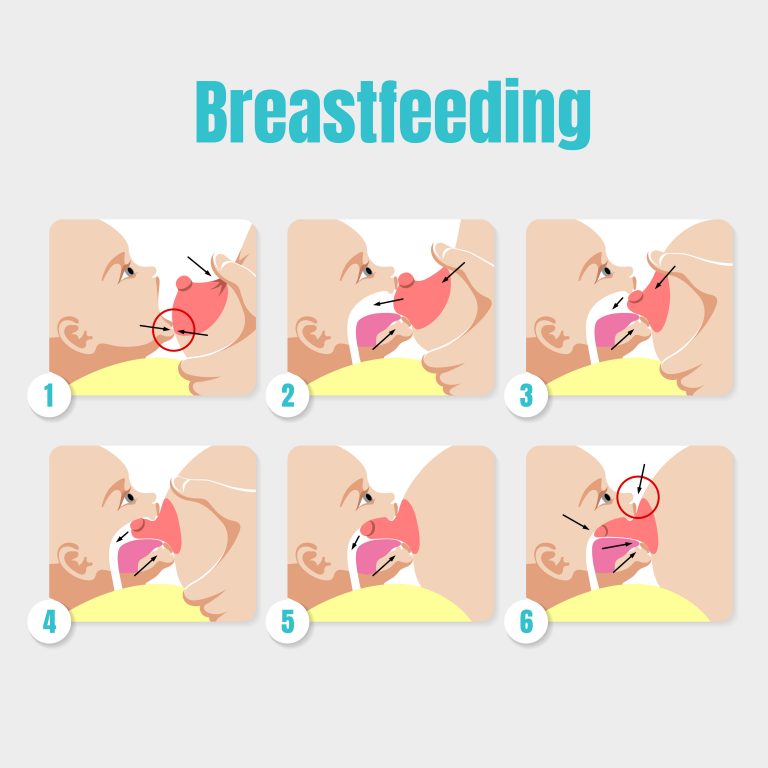
Hand Express Milk
-
How: Gently press around the areola to release a little milk before feeding.
-
Why It Works: Softens nipples for better latching.
-
-
Tool: Use a Haakaa silicone pump for ease.
-
Why It Helps: Simplifies expression.
-
Take Pain Relievers
-
How: Use ibuprofen or acetaminophen, per your doctor.
-
Why It Works: Eases pain and inflammation.
-
-
Caution: Always check with your pediatrician first.
-
Why It Helps: Ensures safety for you and baby.
-
Checklist: Quick Engorgement Relief Tips
-
☐ Nurse or pump every 2–3 hours.
-
☐ Apply warm compress before feeding.
-
☐ Massage breasts gently.
-
☐ Use cold compress after feeding.
-
☐ Hand express to soften nipples.

Long-term Management
Manage breastfeeding engorgement with gentle massage and frequent nursing. Warm compresses relieve swelling. Ensure proper latch for comfort and milk flow.
Managing engorgement while breastfeeding can be challenging. It’s essential to think about how to manage this issue long-term. This means not just dealing with the pain when it happens, but finding ways to prevent it from occurring frequently. What strategies can help you ensure a smoother breastfeeding journey for both you and your baby?
Regular Feeding Schedules
Creating a regular feeding schedule is crucial. Feeding your baby at consistent times helps regulate milk production. This prevents your breasts from becoming overly full, which can cause engorgement.
Think about what feeding schedule works best for you and your baby. You might want to feed every two to three hours during the day. Nighttime might require a different approach based on your baby’s sleep patterns.
Consistency is key. Keeping a journal of your baby’s feeding habits can help you spot patterns and adjust the schedule as needed.
Lifestyle Adjustments
Sometimes, lifestyle adjustments can make a big difference. Consider how your daily habits affect breastfeeding and engorgement.
Stress can impact milk supply and flow. Finding ways to relax and reduce stress can help. Maybe a short walk or a few minutes of meditation each day can make breastfeeding easier.
Diet also plays a role. Staying hydrated and eating well-balanced meals supports healthy milk production.
Think about your clothing choices too. Wearing loose, comfortable bras can reduce pressure on your breasts, minimizing engorgement discomfort.
Could small changes in your daily routine enhance your breastfeeding experience? Reflect on what adjustments might work for you and your family.

When To Seek Help
Experiencing intense pain or fever during breastfeeding signals the need to consult a healthcare professional. Persistent engorgement, redness, or swelling also requires medical attention. Seeking help ensures proper care and prevents complications.
Expert Tips to Manage Engorgement
If engorgement strikes, don’t panic! These expert-backed strategies can help relieve discomfort and get you back to enjoying your breastfeeding journey.
1. Breastfeed Often
Frequent nursing is the most effective way to relieve engorgement. Encourage your baby to feed as often as possible, starting with the fuller breast to promote milk flow.
2. Use Warm Compresses Before Feeding
Applying a warm compress or taking a warm shower before feeding can stimulate milk flow. The warmth helps soften the breast, making it easier for your baby to latch.
3. Try Cold Compresses After Feeding
After nursing or pumping, apply a cold pack (like a gel pack or a bag of frozen peas wrapped in a cloth) for 10–15 minutes to reduce swelling and soothe pain.
4. Hand-Express or Pump Strategically
If your baby can’t latch due to engorgement, hand-express or pump just enough milk to soften your breasts. Avoid over-pumping, as this can signal your body to produce more milk, worsening engorgement.
5. Massage Your Breasts
Gentle breast massage during feeding or pumping can help release milk and relieve blockages. Use circular motions, moving from the outer breast toward the nipple.
6. Use Reverse Pressure Softening
This technique involves gently pressing around the areola to push fluid back into the breast, softening the area so your baby can latch more easily.
How to Manage Breast Engorgement Flowchart
plainShow inline
7. Take Pain Relief (If Needed)
If discomfort is intense, ask your doctor about over-the-counter pain relievers like ibuprofen, which can reduce pain and inflammation. Always check with a healthcare provider before taking medication while breastfeeding.
8. Stay Hydrated and Rested
Dehydration and exhaustion can make engorgement feel worse. Drink plenty of water and rest when you can (we know, easier said than done!).
Checklist: When to Call Your Doctor
-
☐ Fever or chills appear.
-
☐ Red, hot spots on breast.
-
☐ No relief after 48 hours.
-
☐ Baby struggles to latch.
Support Systems
Managing engorgement during breastfeeding involves expressing milk regularly to relieve pressure. Applying warm compresses before feeding can help ease milk flow. Cold packs after feeding may reduce swelling.
Breastfeeding can be a beautiful experience, but it often comes with challenges like engorgement. You don’t have to face this alone; support systems can make a big difference in managing engorgement effectively. Whether it’s leaning on your partner, family, or community resources, each offers unique advantages.
Partner And Family Involvement
Your partner can be your strongest ally during breastfeeding. Encourage them to learn about engorgement and its signs. When they understand what you’re going through, they can offer help without you needing to ask.
Family members can also play a crucial role. Imagine having someone to watch over the baby while you take a hot shower to relieve engorgement pain. Simple acts of kindness, like preparing meals or running errands, can be game-changers during this period. Engaging your loved ones in your breastfeeding journey can lighten your load significantly.
Community Resources
Local community resources can be invaluable. Check if there are breastfeeding support groups in your area. These groups often bring together mothers facing similar challenges, offering a space to share experiences and solutions. You might discover a tip that makes all the difference.
Healthcare professionals can also be part of your support network. Lactation consultants, for instance, can provide specialized advice tailored to your situation. Many hospitals offer breastfeeding clinics—take advantage of them.
Have you explored online communities? Platforms like forums and social media groups can connect you with mothers worldwide. They offer a wealth of shared experiences and advice that could be the key to managing your engorgement better.
How are you leveraging your support systems? The right support can transform your breastfeeding experience from overwhelming to empowering. Don’t hesitate to reach out and build a network that works for you.
Myths And Facts
Breast engorgement can be uncomfortable and challenging. It’s crucial to know both myths and facts for effective management. Proper techniques can relieve swelling and pain, allowing for smoother breastfeeding experiences.
Breastfeeding is a natural process, but it doesn’t always go as smoothly as we might expect. One common issue many new moms face is breast engorgement. It’s an uncomfortable experience, and there’s a lot of misinformation out there. Let’s sift through some myths and facts to help you manage engorgement effectively and keep your breastfeeding journey on track.
Common Misconceptions
Many believe that breast engorgement means you have an abundant milk supply. While it might seem logical, it’s not always true. Engorgement can occur when your body is still figuring out the right amount of milk to produce, leading to too much milk or even a blockage.
Another myth is that you should stop breastfeeding if your breasts are engorged. Some think it will give your body time to adjust. However, this can actually worsen the problem, as milk builds up and increases discomfort. Continuing to breastfeed or express milk is essential.
You might have heard that applying heat to engorged breasts is the best solution. While warmth can provide relief, it’s not always the most effective way to reduce swelling. Cold compresses might actually work better in some cases.
Evidence-based Practices
Research supports breastfeeding on demand as a way to manage engorgement. Feeding your baby whenever they show hunger cues helps regulate your milk supply. It also prevents milk from building up and causing discomfort.
Using a cold compress after feeding can help reduce swelling. Wrap a bag of frozen peas in a cloth and apply it to your breasts. It’s a simple yet effective way to ease the pain and reduce inflammation.
Gentle breast massage before and during feeding can aid in milk flow. Use light pressure and circular motions towards the nipple. This helps release any blocked milk and can make feedings more comfortable for both you and your baby.
Have you ever tried expressing a little milk before feeding? It can soften your breast, making it easier for your baby to latch. This small step can make a big difference in reducing engorgement.
Do you have any tips that have worked for you? Sharing your experiences can help other moms navigate this challenging time. Engorgement is temporary, and with the right approach, you can continue breastfeeding comfortably.
Frequently Asked Questions
Q: How Do You Get Rid Of Engorgement Fast?
A: Apply warm compresses and massage the breasts to improve milk flow. Nurse or pump frequently to relieve engorgement. Use cold packs to reduce swelling. Wear a supportive bra and avoid tight clothing. Consult a healthcare provider if discomfort persists.
Q: Should I Pump To Relieve Engorgement?
A: Yes, pumping can help relieve engorgement by removing excess milk. Use a breast pump or hand express gently. Avoid over-pumping to prevent increasing milk supply. Balance pumping with breastfeeding to maintain comfort and supply. Always consult a lactation expert for personalized advice.
Q: How Long Does Engorgement Last When Breastfeeding?
A: Breast engorgement typically lasts 24 to 48 hours. Frequent breastfeeding can help alleviate discomfort. If symptoms persist, consult a healthcare professional. Proper latching and regular feeding schedules can prevent engorgement issues. Stay hydrated and maintain a balanced diet to support breastfeeding.
Q: How Do You Unblock Engorgement?
A: Apply warm compresses and massage gently to relieve engorgement. Nurse frequently to empty the breasts. Use cold compresses after feeding to reduce swelling. Consider using a breast pump if necessary. Stay hydrated and wear a supportive bra for comfort. If persistent, consult a lactation consultant or healthcare professional.
Q: What causes breast engorgement?
A: Engorgement happens when breasts overfill with milk, often in days 3–5 postpartum as milk transitions, or from missed feedings, per La Leche League. Blocked ducts or oversupply from pumping can also trigger it. Nurse every 2–3 hours to prevent buildup. If pain persists, try warm compresses or consult a lactation consultant to ensure proper milk flow.
Q: How long does engorgement last?
A: Engorgement typically lasts 24–48 hours with proper management, like frequent nursing or pumping, per CDC. If it lasts longer, it may signal blocked ducts or latch issues. Use warm compresses before feeds and cold packs after to ease swelling. If no relief by 48 hours, call your doctor to check for complications like mastitis.
Q: Can I use cabbage leaves for engorgement relief?
A: Yes, chilled cabbage leaves can reduce swelling and pain, thanks to their anti-inflammatory properties, per HealthyChildren.org. Place clean, cold leaves inside your bra for 15–20 minutes after feeding. Change when wilted. Don’t overuse, as they may reduce milk supply. Combine with nursing or pumping for best results.
Q: How can I prevent engorgement when breastfeeding?
A: Prevent engorgement by nursing on demand (8–12 times daily), ensuring a good latch with a Boppy pillow, and pumping only for missed feeds, per American Academy of Pediatrics. Wear a supportive Kindred Bravely bra and wean gradually. These steps keep milk flowing and avoid buildup.
Q: Does engorgement affect my milk supply?
A: Engorgement itself doesn’t reduce supply if managed quickly, per La Leche League. Frequent nursing or pumping prevents your body from slowing production. Untreated engorgement can lead to blocked ducts or mastitis, which may temporarily lower supply. Use a Medela pump to maintain flow and consult a lactation consultant if concerned.
Q: Can I take pain relievers for engorgement pain?
A: Yes, ibuprofen or acetaminophen can ease engorgement pain, but check with your doctor first, per CDC. These are safe for breastfeeding when taken as directed. Combine with warm compresses and massage for faster relief. Always monitor for side effects and avoid overuse to keep you and baby safe.
Q: What should I do if my baby can’t latch due to engorgement?
A: If engorgement flattens nipples, hand express or use a Haakaa pump to soften breasts before feeding, per HealthyChildren.org. Try different positions with a Boppy pillow. If latching remains hard, see a lactation consultant to improve technique. Keep nursing or pumping to prevent worsening engorgement.
Q: Can engorgement lead to mastitis?
A: Yes, untreated engorgement can cause blocked ducts, which may lead to mastitis (breast infection), per CDC. Watch for fever, chills, or red spots. Nurse frequently, massage breasts, and use warm compresses to clear ducts. If symptoms appear, call your doctor for antibiotics or further care to avoid complications.
Q: How can I emotionally cope with engorgement stress?
A: Engorgement can feel overwhelming, but rest, deep breathing, and asking for help ease stress, per HealthyChildren.org. Connect with baby through skin-to-skin time using a Boppy pillow to boost bonding. Join a breastfeeding support group or talk to friends. You’re not alone—small wins like a good feed build confidence!
Q: When should I see a doctor for engorgement?
A: See a doctor if engorgement lasts over 48 hours, you have fever/chills, red hot spots, or baby can’t latch, per CDC. These may signal mastitis or blocked ducts. A lactation consultant can help with latch issues. Track symptoms in a Moleskine journal to share with your doctor. Early help keeps you nursing comfortably.
Conclusion
Managing engorgement during breastfeeding can be challenging but manageable. Remember to nurse frequently. This helps relieve discomfort and prevents complications. Applying warm compresses before feeding can help. Cold compresses after feeding reduce swelling. Gentle massage can ease pressure. Stay hydrated and maintain a balanced diet.
Seek support from healthcare professionals if needed. They offer valuable guidance and reassurance. Practice patience as your body adjusts. With time and care, breastfeeding becomes more comfortable. Prioritize your comfort and baby’s needs. Embrace this journey with confidence and knowledge.
Happy breastfeeding from BestBabyCart.com! Find more tips for your parenting journey.
You are doing a wonderful job.
Taslima Khanam Sultana, a loving mom of three, founded BestBabyCart.com to help new parents navigate the world of baby products with ease. Her passion for making parenting simpler shines through delivering honest, unbiased reviews on must-haves like diapers, strollers, and feeding gear. Taslima’s mission is to empower families with expert tips, ensuring every product is safe and top-quality for your little one. Drawing from her own parenting journey, she’s dedicated to supporting yours!